Home care is, in general, more expensive than care in a doctor’s clinic, as a doctor can attend to many more cases if he or she stays in a central location than if travelling to patients’ homes. For home care to make sense for the doctor, the fees charged must be higher to make up for the shortfall of overall visits. Thus, home care competes on convenience and quality, not on price.
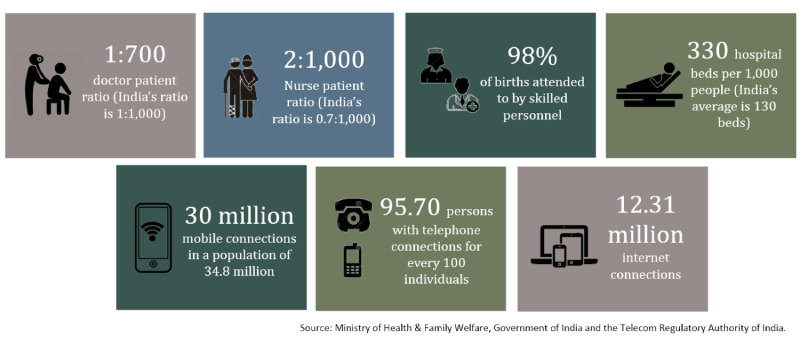
MUrgency’s model expands the provision of primary home care to include non-doctor professionals, allowing home care to compete on both convenience and price. Nurses and emergency medical technicians will be able to offer certain non-medicated and non-invasive services at a lower price than doctors. The platform also allows them greater income potential than what they would make working just in a doctor’s office.
Nurses are a repository of medical skills and training. While they may not have the skills to administer invasive treatments, they are capable of making basic diagnoses, communicating basic information and conducting physical check-ups. They play an important role in monitoring the health of those with more chronic conditions, and recognising when additional treatment is required.
In fact, many of the basic tasks done in a doctor’s office are conducted by nurses, not by the doctor. Nurses and other non-doctor medical professionals can be included in the provision of these services as MUrgency has already developed its medical profession validation process. As it is a resource-intensive process, the ability for nurses to conduct non-emergency care dramatically improves the cost-benefit equation.
Employing nurses and Emergency Medical Technicians to provide non‑emergency care has operational spillover effects. Many in the community were sceptical of receiving medical advice of anyone other than a doctor in an emergency, and indeed several EMTs admitted that they would likely not respond to an emergency when they were not “on-the-job,” for fear that the community would reject their help.
Users do not get a choice of who arrives on the scene to help them in an emergency. This means that a nurse or an EMT could arrive on the scene when the user is expecting a doctor, thus risking rejection by the patient who might choose to wait for the ambulance. This risk increases if the nurse or the EMT lacks documentation that identifies him or her as a medical professional.
However, employing nurses and EMTs to provide consistent non-invasive and non-medicated care builds trust in their skills amongst the community. Thus, when they are called to handle more serious cases, such as medical emergencies, it is expected that the patient will be more trusting of their advice and care.